Not everyone has wisdom teeth, changes in our diet and other factors have influenced the fact that some people never have their wisdom teeth come out.
However, for those that do have them, when they erupt, they can sometimes become infected or impacted, which can cause a lot of discomforts and may even need to be extracted.
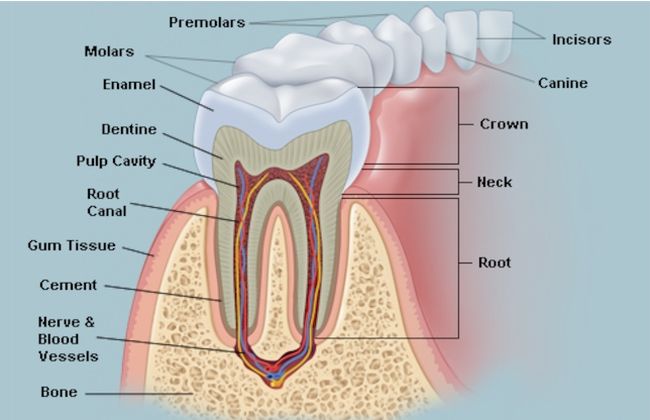
Our adult teeth begin to come out and replace our baby teeth around the age of six. For the most part, the first ones to erupt are the central incisors, then the lateral incisors and the molars. When we are 13 we should have all our adult teeth in place, except the third molars or wisdom teeth.
These third molars are quite unpredictable because one really can’t tell when they will come in or how, or even if they will erupt altogether. There are cases where people only have two, or the whole set of four, or none at all.
If and when the wisdom teeth come out, they can bring a series of problems that include pain, swelling, and inflammation. They tend to erupt between the ages of 17 and 25 years old.
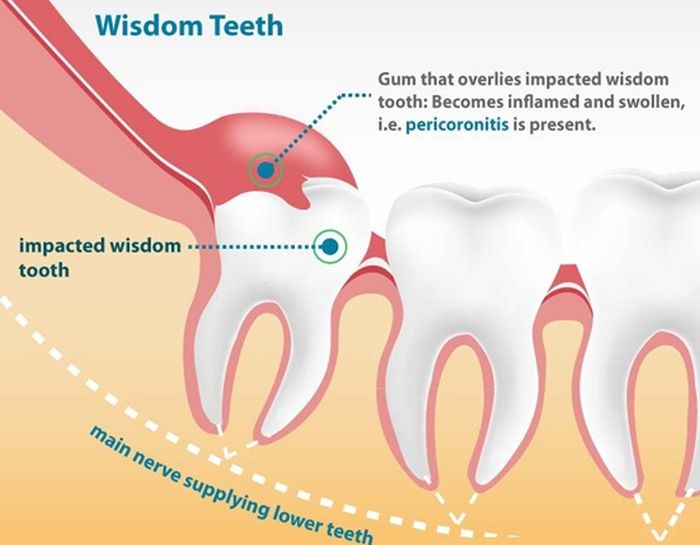
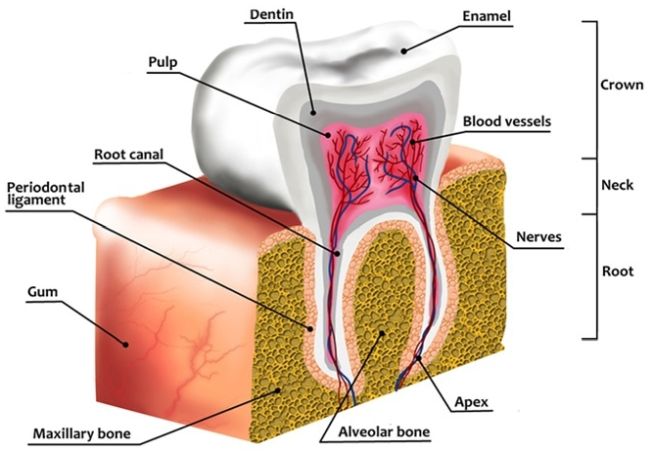
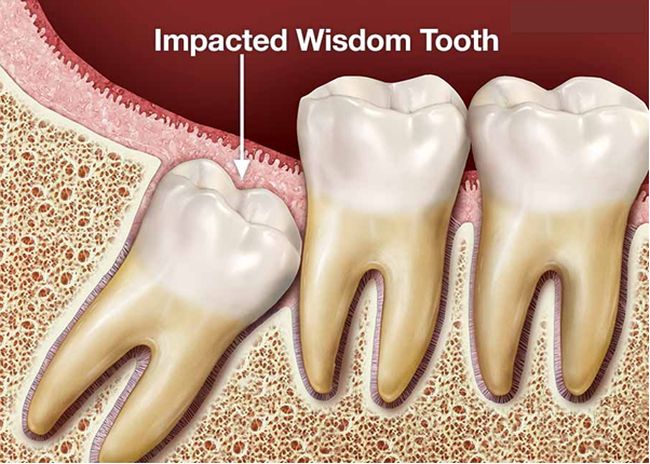 Sometimes they “decide” to come out when our facial features haven’t fully grown, so the third molars don’t have enough space in the jaws, this often results in them coming out at an awkward angle and therefore becoming impacted and/or infected. In these cases, they may need to be extracted.
Sometimes they “decide” to come out when our facial features haven’t fully grown, so the third molars don’t have enough space in the jaws, this often results in them coming out at an awkward angle and therefore becoming impacted and/or infected. In these cases, they may need to be extracted.
But why do we have a third set of molars anyway? As an overall rule, any molars that we have are there to help grind and chew our food. But, since they come in so late in life, they can sometimes present problems if there isn’t enough room for them to erupt.
One of the theories as to why we are having less space in our jaws for these third molars is that our diet has changed quite a bit in the last few generations.
Things like decreased breastfeeding rates, softer foods are given to infants and too little K2 vitamin ingestion have all to do with these morphological changes in our jaws that have caused an underdeveloped jaw in humans.
 How do you know if your wisdom teeth are coming out?
How do you know if your wisdom teeth are coming out?
While you may feel pain when wisdom teeth are coming out, any pain at the back of your jaws isn’t necessarily caused by the emergence of these four teeth.
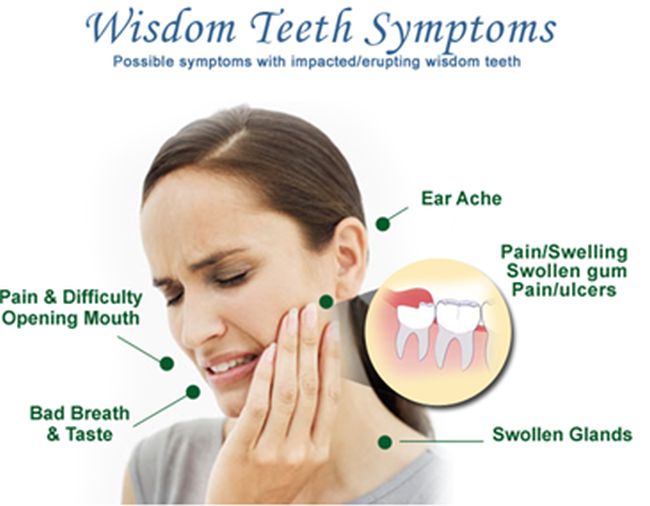
TMJ causes similar symptoms, so check with your dentist for that too. However, watch out for these signs as they may point to third molars wanting to come out:
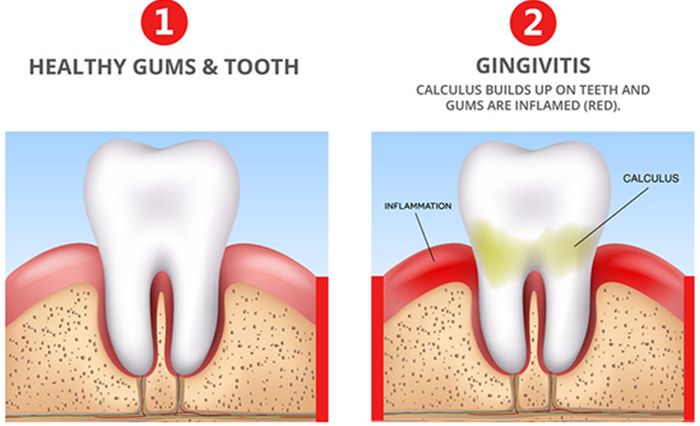
- Swollen gums or visible cuts.
- Pressure or throbbing in the gum area in the back of your jaws.
- Headaches and earaches that are persistent. This happens when they’re trying to emerge but there isn’t enough room, so the pressure that builds up in the neighboring teeth and tissues can cause pain that is sometimes referred to other areas.
- Rinsing and vigorous brushing provide relief.
There’s a common belief that third molars can cause a misalignment in the rest of your teeth, however, there is no real, clinical evidence that this is true.
Why does it hurt when they come out?
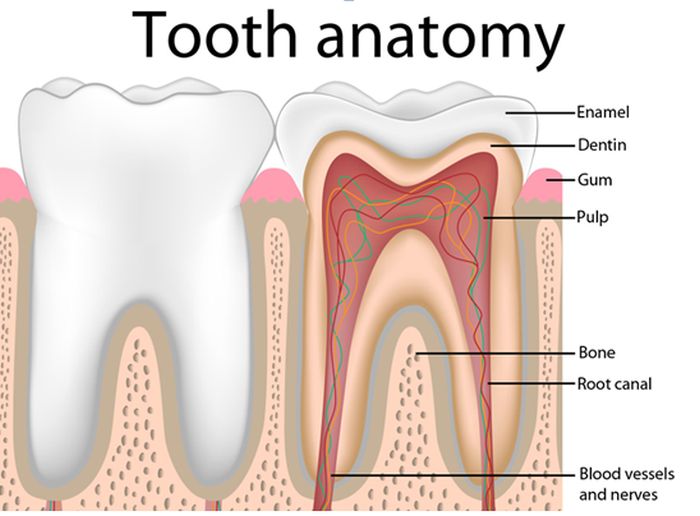
We might not remember it very well, but whenever we had a tooth come out, it hurt. After all, we are having our gums opened by a hard, sharp tooth, and our bone has had to adjust to those changes too, so naturally, it will cause discomfort.
So, wisdom teeth are no exception; but since it happens when are adults, we make a bigger deal out of it. But, there are other reasons why it can cause pain.
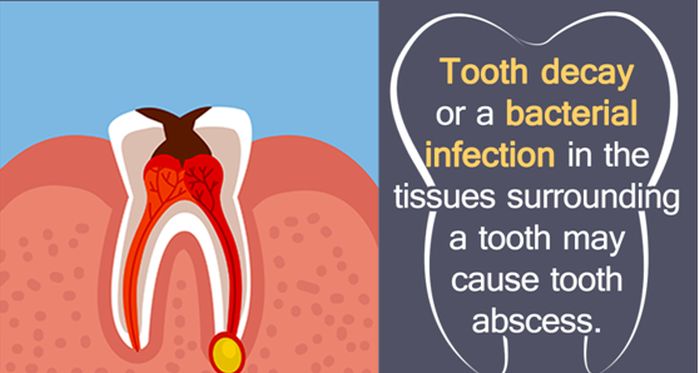
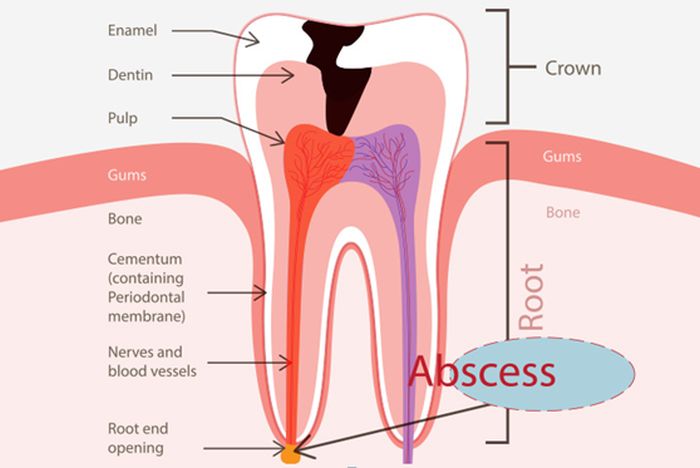
If there isn’t enough room for it to come out, it can try to erupt at an odd angle, sometimes pushing against a neighboring tooth or impacting it, and that can cause pain. If it erupts, but partially, bacteria can enter the area and cause an infection.